So. What is the treatment for CKD?
The short answer is yes, CKD can be treated. It cannot usually be cured. But it can often be stabilised and stopped from getting worse. And there is alot both doctors and you can do. Before we describe that, we need to explain some basics first.
No. Remember that CKD is a spectrum, ranging from mild damage (CKD1-3A) to advanced disease (CKD4-5) where the kidneys fail to work. Most patients have milder form, and will be able to control their CKD with lifestyle changes, medication regular review, by their GP and practice nurse.
However, 1 in 100 patients with CKD will experience progression of their condition despite these measures, and may ultimately require dialysis or a transplant. This equates to 1 in 1000 of the population.
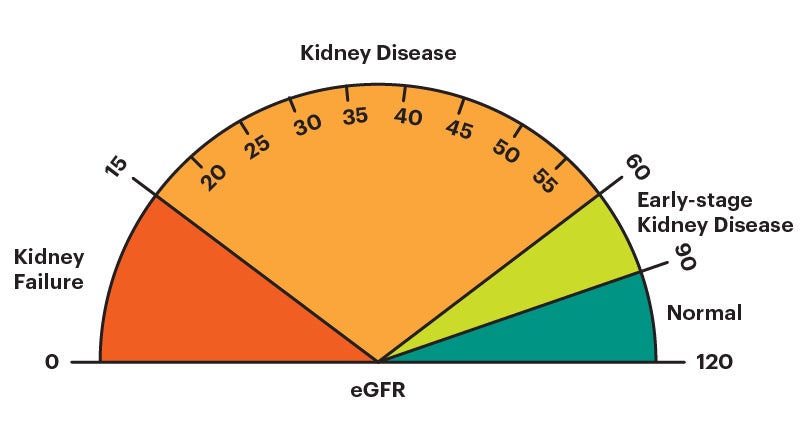
How do doctors decide what to do? They use a classification of severity of CKD (based on something called GFR) to decide upon whether you need treatment. Normal eGFR in humans is 90-120 mls/min. This divides it up into 5 grades:
Notes
– CKD1, 2 and 3A often need little or no treatment.
– CKD3B is worse than CKD3A.
– CKD4 means you may need dialysis or a kidney transplant one day.
– CKD5 means you require dialysis, or a kidney transplant, or supportive care (no dialysis).
This may seem a strange question, as there is no cure for CKD. However, when you are diagnosed with CKD, there are treatments: to help with symptoms; to slow or stop disease progression; and to reduce the risk of heart disease and stroke.
However, despite these measures, 1 in 100 patients will experience progression of their CKD. They may ultimately require dialysis or transplant.
If you need treatment, there are: (1) non-specific CKD treatments (for all causes); and (2) specific CKD treatments (for individual causes). We will now go through the treatment for CKD.
Note. Yes, this will be a lot of tablets, sorry. But they are necessary, to keep you well. And if they contribute to not getting to the next stage (below), they are worth it.
NB. Not all patients will need all of these treatments. If they are needed, you need to be seen regularly by a hospital kidney specialist called a nephrologist.
Is dialysis or a transplant a treatment for CKD?
No, not really. Dialysis can replace about 5% of the function of two kidneys (about 5 ml/min GFR), and a fully functioning transplant 50% (50-60 ml/min GFR). But they do not treat it, i.e. they do not treat the underlying condition that has caused kidney failure.
CKD is not a diagnosis. It is a syndrome with 7 groups of causes/diagnoses. You need to ascertain the underlying cause as this guides treatment. Here are the different treatments for different causes.
1. Unknown
This is the commonest ’cause’, affecting 30% of people with CKD. It is not really a cause, as the phrase means we do not understand the cause. The kidneys usually become small and scarred over the years. It is presumed to be something you are born with, or a late stage of some of the other causes below.
Specific treatment: There is no specific treatment if the cause of CKD is unknown.
2. Diabetes
Both Type 1 and Type 2 diabetes can affect the kidneys. It is called diabetic nephropathy or diabetic kidney disease. It is the second most common cause, affecting 20% of people with CKD. An increased amount of protein in the urine is characteristic. It usually comes on ten years or more, after the onset of diabetes.
Specific treatments:
3. Renovascular disease (RVD)
This is a common cause in older people, especially if they have smoked. It is also known as renal artery stenosis (RAS = tightening of artery to the kidney). It is due to slow long term furring up (with cholesterol and fat etc) of the main blood vessels (arteries) to the kidneys. It is similar to other diseases that are caused by furring up of blood vessels, e.g. heart attacks, and strokes.
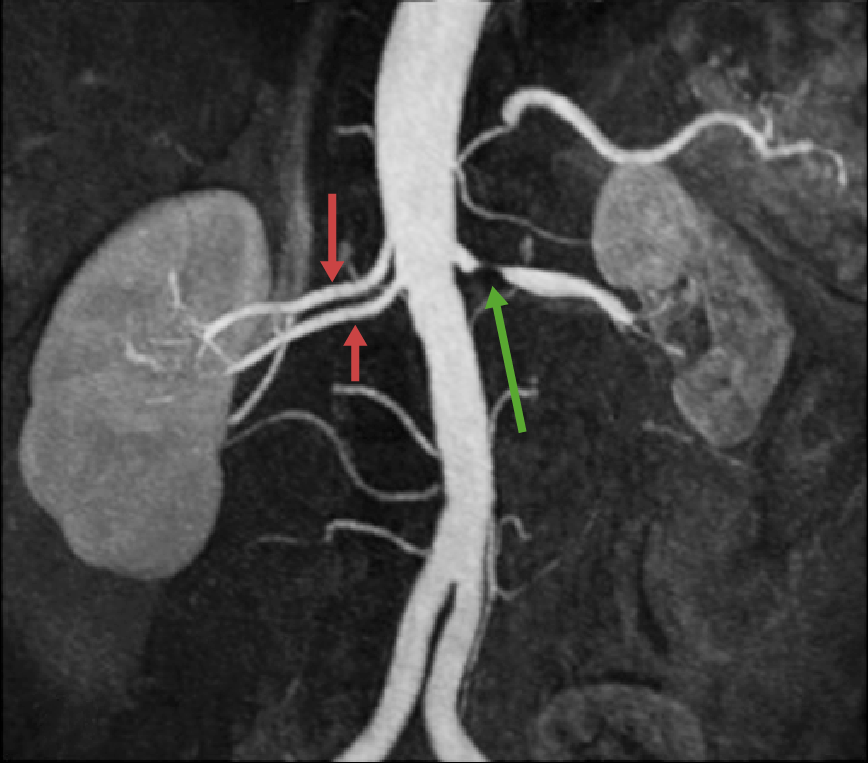
This is a special x-ray called an angiogram that shows a Left renal artery stenosis (green arrow) with two normal renal arteries on the Right. This is a normal variant and quite common (25% of the population)
Note. Some people have more than one cause of CKD. For example, it is quite common for people with diabetes to have diabetic kidney and renovascular disease.
Specific treatments
4. Chronic glomerulonephritis (‘GN’)
This is an inflammation of the kidney’s filtering units (glomeruli; one million in each kidney). There are 7 subtypes. All are considered an ‘auto-immune’ disease, i.e. something has aggravated the body’s immune (defence) system.
And the immune system is attacking the glomeruli and/or small blood vessels within the kidney. Some of this group are called a ‘vasculitis’. They are similar. For most types, an increased amount of protein in the urine is characteristic.
Specific treatments
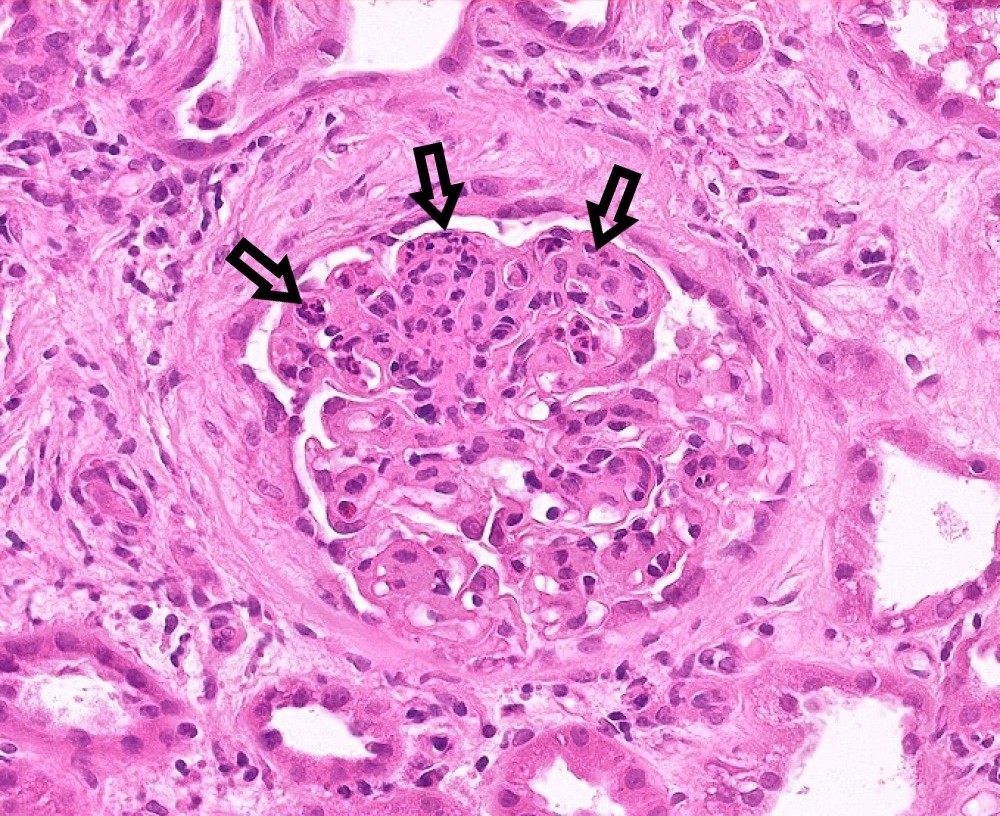
This is a glomerulus (trust us, it is!) one of the million tiny filtering units in each kidney. This one is affected by a type of glomerulonephritis called IgA nephropathy, the commonest type. The arrows point out the affected areas.
5. Polycystic kidney disease (PKD)
This is the only common inherited cause of chronic kidney disease. There are many cysts in both kidneys. It is not really a kidney disease. It can affect the body in many other ways, e.g. cysts in the liver, and other abnormalities in the heart and brain. If you have it, so will 50% of your children.
Specific treatments
6. Obstruction of the urinary tract (kidneys, ureter or bladder)
Both kidneys have to be blocked to cause CKD. Common causes include an enlarged prostate (in a man) and some pelvic cancers (especially in women). Kidney stones rarely block both kidneys. This is the most treatable cause of CKD. So it is very important to make the diagnosis.

Blockage of the left kidney and ureter (tube from the kidney to the bladder). As the other side is not blocked, CKD would not occur
Specific treatment – the kidneys need to be unblocked. This can be done in a variety of ways including the insertion of a catheter (tube) into the bladder; or x-ray or sound treatments (including removing stones) – and operations on the prostate gland (in a man).
7. Chronic tubulointerstitial disease (TID)
This is an inflammation of the kidney’s tubules and surrounding structures. It is a group of diseases with several causes, including:
– Vesicoureteric reflux nephropathy (or ‘reflux’) – is a condition that causes urine to back up into your kidneys, and cause recurrent urine and kidney infections. This affects women more than men, and can be inherited in a complicated way
– Drugs – e.g. aspirin and similar drugs (NSAIDS), and lithium
– Sarcoidosis – and other rare kidney diseases we do not really understand.
Specific treatments (these depend on the cause, and are very different depending on that cause):
For most people the answer is ‘no’. People with milder forms – called CKD1, CKD2 and CKD3A – do not need to be referred. Patients with CKD3B should be discussed with a kidney specialist (called a ‘nephrologist’ or ‘renal physician’).
But. If you have more serious CKD – i.e. CKD4 or CKD5 – your GP should refer you to one of them. You should see a senior doctor, either a consultant (boss), or their deputy called a registrar.
It is important not to be discharged until your CKD is stable. If you are discharged, the hospital specialist needs to give you and your GP a clear monitoring plan, and criteria for referral back. Keep the name of your consultant and his/her secretary’s name, number and email address.
Nonetheless, it is important to stay positive about it. If you are seeing a hospital specialist you can really help by keeping good communication going between them and your GP, especially as computer systems don’t always link up.
[“Yeah, thanks, we have spotted that!” Ed]
We have described treatment for CKD. There is alot doctors and you can do. We hope it has helped you.
[“Wo. That’s complicated.” Ed] Yes, it is, sorry.
If your CKD is due to obstructive nephropathy (blocked kidneys) or glomerulonephritis, there are very effective treatments. So it is important your doctors look hard for these with the investigations above – especially the kidney ultrasound and immunology blood tests.
This article was reviewed by Dr Vicki Ayub, Consultant Nephrologist, UHCW Coventry.