So. What is about haemodialysis (HD)? Let’s start with the basics.
Dialysis is a treatment to remove waste products and fluid from your blood. It is needed when chronic kidney disease (CKD) has progressed to a point when your own kidneys can no longer do this. This is called CKD Stage 5, i.e. kidney failure.
Dialysis is one (very important) aspect of your care, but it is only part of your total treatment. There are tablets and injections (like erythropoietin, EPO) that are very important as well.
Peritoneal dialysis and haemodialysis are the two main types. Both types provide about 5% kidney function. In this way, they do not ‘cure’ kidney failure, just control it – by replacing some of your kidney function. Most patients start to feel a bit better three months or more after starting dialysis.
When kidneys reach CKD5, they rarely recover. Dialysis is usually permanent (or until you have a transplant).
In haemodialysis, a machine removes blood from your body, filters it through a dialyser (artificial kidney) and returns the cleaned blood to your body. This is a 3-5 hour treatment, and most patients have it for 4 hours three times a week. Even though the session is usually four hours, the process will take 6-8 hours of your day.
Most patients will also be asked to follow a fluid restriction of 1.5 litres a day, or less. This can be very hard.

Patient connected to haemodialysis machine. Dialyser is within the machine.
No. The dose depends on your size. Smaller people may need three hours, 2 times a week; and large people five hours, 4 times a week.
It can take place in:
For 1 and 2, you will be given some regular ‘slots’ (days/times) to do it – e.g Monday/Wednesday/Friday morning, or Tuesday/Thursday/Saturday afternoon. There are usually three sessions a day, morning, afternoon and evening.
Before you can start haemodialysis, you will need to undergo a minor surgical procedure to create (vascular) ‘access’ to the bloodstream. This may be a:
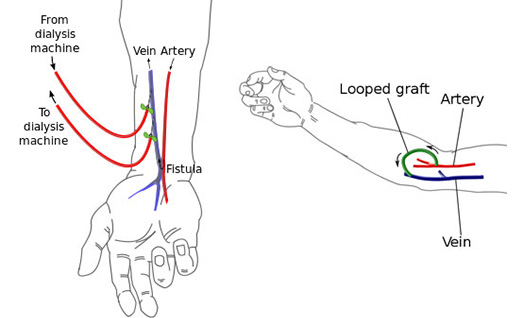 Fistula (left) and Graft (right)
Fistula (left) and Graft (right)
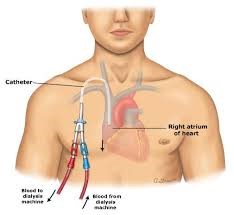
Central venous catheter (‘line’)
With AV fistulas and grafts, the connected artery and vein enlarge, which makes dialysis access easier. When larger, this helps blood flow in and out of your body faster. This is required for good dialysis.
Whichever you have, we call it your ‘access’. And you need to look after it. For example, please do not let anyone take blood or your blood pressure from your fistula or graft arm.
There is usually a wait of up to 30 minutes as the nurses clean the machine from the previous patient. The wait may be longer if you use hospital transport (see below).
When the nurses are ready, two needles are inserted into the fistula (or graft) and you are attached via tubes to the machine; or if you have a line, the lines two tubes are attached to the machine.
 Patient on haemodialysis through a fistula
Patient on haemodialysis through a fistula
The needles are placed in the fistula, with the dialyser just above the middle of this person’s arm
Some people experience low blood pressure during or immediately after haemodialysis. This may make you feel nauseous, dizzy or faint.
You will wait about 30 minutes after a session (longer if you use hospital transport, see below), as the nurses need to check you are OK before you go home.
Narrowing. Fistulas can slowly narrow (forming a ‘stenosis’). There are usually warning signs before blockage, such as difficulty needling, poor flows through the access, or extended post-dialysis bleeding when the needles have been removed.
If this happens the veins should be checked for a narrowing. This will involve an ultrasound scan of your fistula. If there is a narrowing in your fistula this can be treated by having a ‘fistuloplasty’ procedure, in the x-ray department. A fistuloplasty is a procedure where a wire and then balloon are inserted into the fistula to stretch the narrowing in the vein or artery.
Blocking. If a blood clot blocks your fistula completely, you will not be able to feel the ‘buzz’ of the fistula. If this happens, you need to call your renal team urgently, and go to the hospital. A rapid x-ray procedure or operation is needed to remove the blood clot and get the fistula working again. This is more likely to work if you seek help urgently.
Blockage. Lines can also block. If your line blocks, it may be possible to unblock it with a ‘clot busting’ drug, or to replace it with a new one. The nursing staff can apply these to the line whilst you are present in the dialysis unit.
Infection. Lines can get infected. Keeping a clean dressing over the line reduces the chances of infection. Infection on the line can show itself as either pus (a dirty discharge on the dressing) around the entry point of the line; or blood poisoning with fever and shivers on dialysis. Intravenous (IV) antibiotics will be required. If they do not work, the line will have to be removed.
Patients may drive themselves to have dialysis, or be brought by family or friends. There are usually designated free parking spaces close to the hospital or satellite unit. We would encourage you to travel independently if possible. Why? It is more convenient, and you will not have to spend time waiting for transport.
If you (or family) are not able to bring you up to the hospital (or satellite unit) for dialysis, the renal team will arrange hospital transport for you. Hospital transport drivers need to transport other patients not necessarily from your area, so you will be sharing the transport. Therefore they can take quite a long time to drive to and from the hospital, as several patients will need be picked up and taken home.
Less work for you
Easier to increase dialysis dose
Company of other patients at the dialysis sessions
Easier to get nurses and doctors to see you.
Independence
Travelling easier (no travelling required)
Can drink more
As it is continuous, its more like normal kidneys.
We have described what is haemodialysis (HD). It is not an easy life for a patient, but it is effective and can keep you alive for many years.
If your fistula has stopped (or you think it might do) go to the nearest kidney hospital urgently. You may well need an urgent procedure or operation to get it going, and time is of the essence.