Here are 10 facts abut vasculitis.
 Henoch-Schönlein purpura
Henoch-Schönlein purpura
1. Definition: Vasculitis refers to inflammation of blood vessels, which can cause damage to the vessels and affect various organs. It can affect blood vessels within individual organs, or all blood vessels in the body.
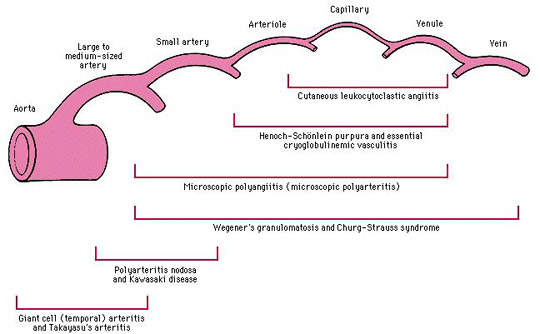
Types: There are several types of vasculitis, including:
2. Causes: Vasculitis can be caused by (or associated with) infection, certain medications, autoimmune disorders, or cancer.
3. Risk factors: Include genetic predisposition, infections such as hepatitis B and C, certain medications like hydralazine and propylthiouracil, and underlying autoimmune disorders such as rheumatoid arthritis or lupus (SLE).
5. Diagnosis: Diagnosis involves a combination of clinical assessment, bloods tests (e.g. inflammatory markers; immunology, including ANCA), and imaging (CXR, CT/MRI) or pathological studies (e.g. angiography, biopsy).
Monitoring: Regular monitoring of disease activity, organ function, and treatment side effects is crucial for managing vasculitis.
Classification criteria: The American College of Rheumatology (ACR) and the Chapel Hill Consensus Conference (CHCC) have established criteria for classifying different types of vasculitis.
6. Treatment: Treatment depends on the underlying cause and severity, and may involve corticosteroids, immunosuppressive medication, or biological agents. All have side effects.
7. Complications: Untreated vasculitis can lead to complications such as death, organ damage (that can be severe, e.g. dialysis), aneurysm formation, or increased risk of infection.
10. Referral (Multidisciplinary care required). Vasculitis management often requires a multidisciplinary approach, involving rheumatologists, nephrologists, dermatologists, and other hospital-based specialists.