Gallstones: Causes, Symptoms, Treatment
In this article, we will describe 10 facts about gallstones. It is largely for health professionals.

Key Points
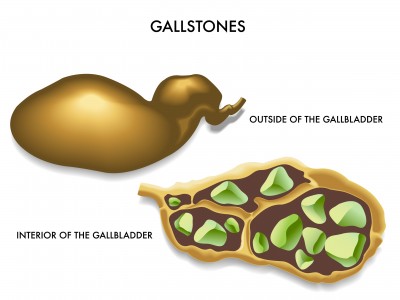
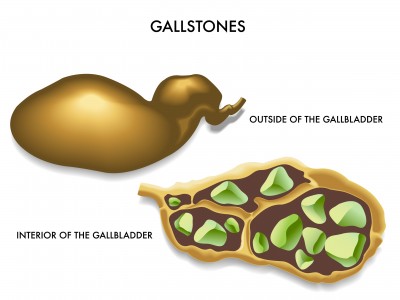
- Definition: Gallstones are solid deposits that form in the gallbladder and may lead to biliary colic or more serious complications, including cholecystitis and pancreatitis.
- Content: They are made up of cholesterol, bilirubin, and calcium salts.
- Symptoms: They are often asymptomatic but can cause upper pain (especially on the right) or obstructive symptoms (jaundice) when they block the bile ducts.
- Diagnosis: Is typically confirmed via ultrasound, and treatment options range from watchful waiting to surgical removal of the gallbladder.
- Risk factors: Include age, female gender, obesity, and certain dietary factors.
1. Definition
- Gallstones, or cholelithiasis, are crystalline deposits that form in the gallbladder, usually composed of cholesterol, bilirubin, or a combination of both.
- When gallstones migrate and obstruct the cystic or common bile duct, they can cause pain (biliary colic) and lead to complications like cholecystitis, cholangitis, or pancreatitis.
2. Epidemiology
- Gallstones are common, affecting about 10–15% of adults in the UK.
- They are more prevalent in women, with a female-to-male ratio of approximately 2:1.
- Gallstone incidence increases with age, and although most gallstones remain asymptomatic, about 20% of affected individuals will develop symptoms or complications.
3. Risk Factors
Several factors increase the risk of gallstone formation:
- Gender: Women are at higher risk, especially during reproductive years.
- Age: Gallstone prevalence rises significantly after age 40.
- Obesity: Excess body weight increases cholesterol levels in bile.
- Rapid Weight Loss: Fasting or rapid dieting promotes gallstone formation.
- Pregnancy: Hormonal changes during pregnancy slow bile flow and increase gallstone risk.
- Genetic Factors: A family history of gallstones can increase individual risk.
- Ethnicity: Certain populations, such as Native Americans, have higher prevalence.
- Dietary Factors: High-fat diets or low-fiber intake may increase risk.
- Other Conditions: Diabetes, liver cirrhosis, and hemolytic anemia are linked to a higher incidence of gallstones.
4. Causes
Gallstones form when the balance of substances in bile – cholesterol, bile salts, and bilirubin – becomes disrupted. This can occur due to:
- Cholesterol Supersaturation: When there is too much cholesterol relative to bile salts, cholesterol crystals form, leading to cholesterol gallstones.
- Bilirubin Excess: Certain conditions (e.g., hemolytic anemias, liver cirrhosis) cause high bilirubin levels, forming pigment stones.
- Bile Stasis: Conditions that reduce gallbladder contraction (e.g., prolonged fasting or pregnancy) promote bile stasis and stone formation.
5. Symptoms
Gallstones are frequently asymptomatic. However, when they cause symptoms, presentations include:
- Biliary Colic: A steady, intense pain in the right upper quadrant (RUQ) or epigastrium, often radiating to the right shoulder blade. Pain is typically triggered by fatty meals and lasts from minutes to hours.
- Nausea and Vomiting: Common in cases of biliary colic or cholecystitis.
- Fever and Chills: Seen in acute cholecystitis or cholangitis.
- Jaundice: Indicative of bile duct obstruction or choledocholithiasis (stone in the common bile duct).
6. Diagnosis
Diagnosis is often clinical, supported by imaging:
- History and Physical Examination: RUQ tenderness, Murphy’s sign (pain on palpation of RUQ during inspiration), and fever may suggest cholecystitis.
- Ultrasound: First-line imaging modality, with high sensitivity for detecting gallstones, particularly in the gallbladder.
Investigation
Additional investigations may be required in complicated cases:
- Liver Function Tests (LFTs): Elevated alkaline phosphatase (ALP) and bilirubin may suggest bile duct obstruction.
- Complete Blood Count (CBC): Leukocytosis may indicate infection (cholecystitis or cholangitis).
- Amylase/Lipase: Raised levels can indicate pancreatitis, often due to a gallstone obstructing the pancreatic duct.
- Endoscopic Retrograde Cholangiopancreatography (ERCP): Both diagnostic and therapeutic, ERCP is used to locate and remove common bile duct stones.
- Magnetic Resonance Cholangiopancreatography (MRCP): A non-invasive imaging alternative to ERCP for detecting bile duct stones.
Differential Diagnosis
Other conditions to consider in patients with RUQ or epigastric pain include:
- Peptic Ulcer Disease: Often presents with burning epigastric pain, related to meals.
- Gastroesophageal Reflux Disease (GERD): Causes epigastric discomfort, often associated with acid regurgitation.
- Acute Pancreatitis: Severe epigastric pain radiating to the back, associated with raised amylase/lipase.
- Acute Appendicitis: Pain may initially present as periumbilical but migrates to the right lower quadrant.
- Hepatitis: RUQ discomfort with jaundice, and significantly elevated transaminases.
7. Treatment
The approach to treatment depends on symptom severity and the presence of complications:
- Asymptomatic Gallstones: Usually managed with observation, as the risk of progression to symptomatic disease is low.
- Symptomatic Gallstones (Biliary Colic):
- Cholecystectomy: Elective laparoscopic cholecystectomy is the definitive treatment for recurrent biliary colic.
- Pain Management: NSAIDs are often effective; opioids may be necessary for severe pain.
- Complicated Gallstones:
- Acute Cholecystitis: Intravenous (IV) antibiotics (e.g., ceftriaxone plus metronidazole), fluid resuscitation, and urgent cholecystectomy (ideally within 72 hours).
- Choledocholithiasis: Managed with ERCP to remove common bile duct stones, followed by cholecystectomy.
- Cholangitis: An emergency; treatment includes IV antibiotics, biliary decompression via ERCP, and eventual cholecystectomy.
- Gallstone Pancreatitis: Managed with supportive care (fluids, analgesia), ERCP for ductal obstruction if required, and delayed cholecystectomy to prevent recurrence.
8. Complications
Gallstones can lead to several complications, especially if untreated:
- Acute Cholecystitis: Infection of the gallbladder, often requiring emergency intervention.
- Choledocholithiasis: Stones in the common bile duct, leading to jaundice or cholangitis.
- Cholangitis: Life-threatening infection of the biliary tree, requiring urgent decompression.
- Gallstone Pancreatitis: Caused by obstruction of the pancreatic duct, which can lead to severe inflammation.
- Gallbladder Empyema or Gangrene: Infection can progress to pus formation (empyema) or tissue death (gangrene) in the gallbladder.
9. Prognosis
- The prognosis for uncomplicated, asymptomatic gallstones is generally excellent, as they rarely progress to complications.
- Symptomatic gallstones managed by cholecystectomy have a good prognosis, with most patients experiencing complete symptom resolution.
- However, the prognosis is guarded in cases of severe complications like cholangitis or gallstone pancreatitis, especially if treatment is delayed.
10. Prevention
Preventive strategies focus on modifiable risk factors:
- Healthy Diet: A diet high in fiber and low in saturated fats may reduce gallstone risk.
- Weight Management: Avoid rapid weight loss; gradual weight reduction is preferable.
- Physical Activity: Regular exercise may help prevent obesity and reduce gallstone risk.
- Avoiding Prolonged Fasting: Regular meals help maintain normal bile flow and prevent stasis.
Summary
We have described 10 facts about gallstones. We hope it has been useful.