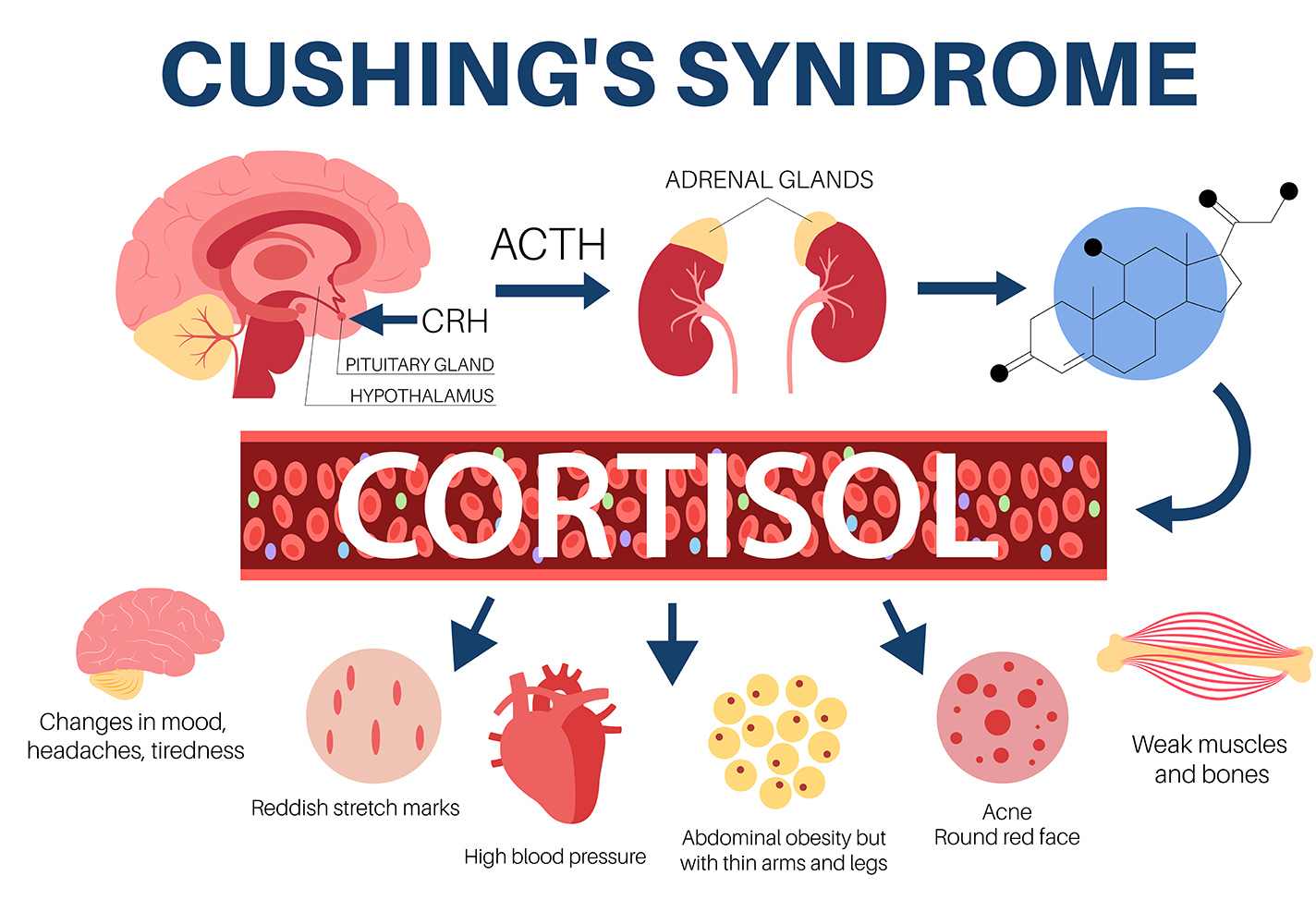
1, Definition: Cushing’s Syndrome is a rare endocrine disorder caused by excess levels of cortisol in the body, either due to exogenous steroid use or overproduction by the body.
2. Causes: The most common cause is iatrogenic (medication-induced), while endogenous causes include pituitary tumours (Cushing’s disease), adrenal tumours, or ectopic ACTH-producing tumours.
3. Risk Factors: Risk factors for endogenous Cushing’s Syndrome include family history of endocrine disorders, certain genetic syndromes (e.g. MEN1), and female sex.
4. Symptoms: Classic symptoms include weight gain (central obesity), moon face (moon facies), buffalo hump, purple striae, hypertension, and diabetes.
5. Diagnosis: Diagnosis involves confirming hypercortisolism through 24-hour urine free cortisol, low-dose dexamethasone suppression test, or midnight salivary cortisol. Further testing (e.g. ACTH levels, imaging) determines the underlying cause.
6. Treatment: Treatment depends on the cause:
8. Prognosis: Prognosis varies depending on the underlying cause and treatment effectiveness. Patients with successfully treated benign tumours generally have a good prognosis, while those with malignant tumours or uncontrolled cortisol levels may experience significant morbidity.
9. Prevention: Prevention focuses on judicious use of glucocorticoids and monitoring for signs of Cushing’s Syndrome in patients on long-term steroid therapy.
10. Referral: Refer patients with suspected or confirmed Cushing’s Syndrome to an endocrinologist for further evaluation and management.