This is how the AI article summary could look. Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat.
10 Questions to Ask Your Kidney Doctor About CKD
Here are some questions you might consider asking your kidney doctor about Chronic Kidney Disease (CKD).

“All questions are good questions”
1. What stage is my CKD, and what does that mean for my outlook?
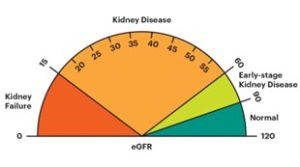
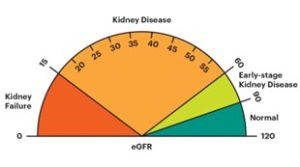
- There are 5 stages in the CKD classification.
- The CKD stage describes the severity of the chronic kidney disease; the higher the grade (stage), the worse the kidney function – the higher the stage, the more likely it is you will need dialysis one day
- The 5 stages are based on something called ‘GFR’ (glomerular filtration rate). Normal GFR is 90-120 mls/min
- GFR is a blood test which estimates the level of function of the kidney – the higher the GFR, the better the kidney function (and therefore the lower stage of CKD that the patient will be in).

5 stages of CKD
Notes
- Fortunately only 1 in 100 of people with CKD ever need dialysis or a kidney transplant – equating to 1 in 1000 of the population
- Only patients with Stage 3B or higher need to have a kidney doctor. Some of these (CKD3b-4) can be discharged back to their GP, if kidney function stable.
2. What is the cause of my CKD, and can it be managed?
- Write it down. Ask them the doctor to explain it, and recommend where to go for further information
- CKD is not a diagnosis. It is a syndrome with 7 common causes (diagnoses):
- The most common (30%) ’cause’ is unknown; often with small kidneys on an ultrasound. The most common known cause is diabetes (20%)
- It is important to diagnose a glomerulonephritis (kidney inflammation) as many are controllable with tablets that suppress the immune system
- It is also important to diagnose obstructive nephropathy (blocked kidneys) as it is often reversible with a catheter (tube) placed in the bladder
- The other 3 causes are: polycystic kidney disease (PKD), tubulointerstitial and renovascular disease
- Many patients have more than one cause. I.e. the ’cause’ is multifactorial.
3. How will CKD affect my daily life, and are there any lifestyle changes I should make?
At its earlier stages (CKD1-3A) it will not have a huge effect on your life. At CKD4-5, it will. Ask what you can expect.
4. What medications are available to slow CKD progression, and what are their potential side effects?
- Blood pressure tablets called Angiotensin-Converting Enzyme (ACE) inhibitors or Angiotensin Receptor Blockers (ARB), along with Sodium-Glucose Cotransporter-2 inhibitors (SGLT2i) (in combination), significantly slows the progression of Chronic Kidney Disease (CKD) in patients with and without diabetes
- ACE/ARBs may increase the blood potassium level, which therefore needs to be monitored.
5. Are there any dietary restrictions or recommendations for someone with CKD?
- In the early stages of CKD, there is usually no ‘special diet’.
- If your CKD advances you may want to see a renal dietitian for advice on how to support your nutritional needs
- But in general, avoid foods that are high in sodium. Too much sodium can cause high blood pressure and therefore be bad for your kidneys
- Some people with kidney disease may to restrict the intake of potassium and protein, as they both put more pressure on the kidneys. Ask your kidney doctor (nephrologist), specialist nurse or dietitian.
6. How often should I have my kidney function monitored, and what tests will I need?
It depends on the stage of CKD you are in:
- CKD1-2 – GFR/creatinine every 12 months
- CKD3A – GFR/creatinine every 6 months
- CKD3B – GFR/creatinine every 4-6 months
- CKD4 – GFR/creatinine every 2-4 months
- CKD5 (before dialysis) – GFR/creatinine every 1-2 months.
7. What signs or symptoms I should watch for that might indicate CKD progression?
Here are 10 of the most common symptoms of CKD (usually start at Stage 3B CKD):
- Urinary symptoms – relatively rare (surprisingly). Foamy urine can be a sign of CKD with increased protein in your urine
- High blood pressure (BP) – most people with CKD have high blood pressure
- Shortness of breath and ankle swelling (red flag symptoms) – you need to see a doctor soon
- Tiredness
- Pain – while body (especially bone) pain
- Muscle weakness
- Not being hungry – poor appetite, especially with food that has little taste (or tastes metallic)
- Itching – whole body
- Poor concentration and sleeping
- Other (non-specific) – including a feeling of deep cold, leg cramps and restless legs.
8. Can CKD lead to other health issues, such as heart disease or bone disease?
- Yes. CKD affects the heart and the bones. But there is good medication to treat both
- If you have other long-term conditions (e.g. high blood pressure, diabetes, heart failure), they all need to be controlled
- If not, they can worsen your CKD. If you need to see another specialist in those areas, ask your GP (or kidney doctor) to refer you to one.
9. What are my treatment options if CKD progresses to end-stage renal failure (ESRF; also called kidney failure or Stage 5 CKD)?
- For advanced Chronic Kidney Disease (CKD5), you have three main treatment options: a kidney transplant, dialysis (either haemodialysis or peritoneal dialysis), or supportive (conservative) management (not having dialysis or a transplant)
- A kidney transplant is often the preferred option for eligible patients, offering better quality of life and life expectancy, but dialysis is a necessary alternative or bridge until a transplant is possible
- Dialysis is a technique to filter your blood (like normal kidneys), while a kidney transplant involves surgery to replace the diseased kidney with a healthy one.
10. Are there any clinical trials or new treatments for CKD that might be suitable for me?
If there are none based at the kidney unit you are attending, ask if any other units are recruiting.
You may also want to ask your doctor about managing related
health conditions, such as diabetes or hypertension, and how they impact your CKD.
Be proactive and protect your kidney health.